
A spinal cord stimulator (SCS) is a device that is placed under the skin of the patient through a surgical procedure. It is used to decrease pain in the spine.
The spinal cord stimulator (SCS) device generates a mild electric current to the spinal column. Thin wires transmit the electric current to the nerve fibres of the spinal cord from a pulse generator. When the current is turned on, the SCS starts stimulating the nerves in the area where the patient feels pain. Pain decreases as the electrical pulses alter and mask the pain signals from reaching the patient’s brain.
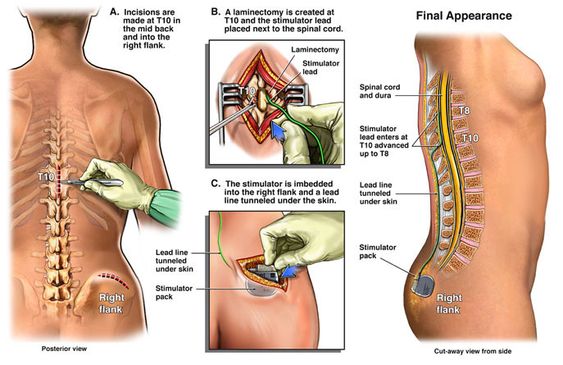
Spinal cord stimulators comprise of electrodes and a small pacemaker like device known as the generator. The electrodes are placed between the epidural space (the vertebrae) and the spinal cord. The generator is positioned under the patient’s skin, typically near the abdomen or the buttocks. The spinal cord stimulator generates electrical impulses with the help of a remote control when patients feel pain. The remote and its antenna are outside the patient’s body.
SCS is mostly used if post-surgical pain treatment options have failed to deliver any significant relief to the patient. SCS may be used to treat the following types of chronic pain:
Spinal cord stimulation helps enhance the patient’s overall quality of life. It improves sleep and decreases the need to take pain relief medication.
Patients that experience the following symptoms can be a good candidate for undergoing SCS:
Following are the main 3 types of spinal cord stimulators:
This consists of a battery placed in the patient’s spine through a surgical procedure. When the battery runs out, it must be replaced through another procedure. This can be more beneficial for patients with pain in only one body part as they need less energy to manage their pain.
This involves a battery that is implanted in the patient’s spine during surgery. The patient can also recharge the battery without needing another surgery. As the energy source is rechargeable, these simulators can generate more amount of electricity. This is best for lower back pain or pain in one or both legs.
This type of stimulator is a traditional design. It involves a battery that is outside the patient’s body. This simulator is not used much nowadays as newer and better technology is available. This simulator has rechargeable batteries. However, similar to the rechargeable implantable pulse generators, this one may be a good choice for patients with lower back and leg pain because of the power of the device.
This surgery is performed in a hospital in the ambulatory surgery unit.
Firstly, the patient will receive anaesthesia. Then an epidural needle is placed into the epidural space with the help of x-ray guidance.
After placing the needle properly on the required location, a small electrode is inserted through the needle into the epidural space (vertebras) in the spine. This process is then repeated as most of the trials require the two-electrode placement. This is known as the spinal cord stimulator trial.
The rest of the procedure is then performed under the effect of general anaesthesia. The surgeon will make a small incision in the lower back of the patient for the electrode placement, as highlighted in the trial. The electrodes are secured to the bone of the spine and the ligaments.
The pulse generator or the battery is then implanted underneath the patient’s skin over the buttock area. The electrodes are then tunneled under the skin and connected with the pulse generator.
All incisions are closed carefully.
After the follow-up appointments and the first two weeks post-surgery, the patient can gradually increase the level of activity. Many patients are able to return to normal routine in nearly 6-8 weeks post-procedure.
Some of the side effects associated with the procedure include:
SCS cannot cure any condition that is causing pain. Instead, it just helps patients manage their pain. SCS is considered successful if at least 50% of the pain is resolved.
Various studies of spinal cord stimulation demonstrate good to excellent (50 to 80%) long-term relief in patients suffering from chronic pain.
The sooner the patient starts moving and returning to normal activity, the better. Many patients have reported that once they get used to the device placed in their body and learn to use it, they experience much less pain. Some patients even say that the discomfort also lessens to nearly 50 to 70%.
The units are moveable and permit an incredible degree of freedom to the patient. Patients who have SCS implanted are able to swim, run and easily carry out daily activities that previously had created a lot of problems due to the pain they experienced.
Yes, the spinal cord stimulation procedure is covered by many major health insurers. This includes Medicare, commercial payers, and most workers’ compensation programs.
A study published in 2015 named “Predictors of spinal cord stimulation success” demonstrated that spinal cord stimulation led to statistically significant and meaningful pain relief in nearly 50-70% of selected patients. Also, a study conducted in 2016 named “Patient Outcomes and Spinal Cord Stimulation” demonstrated that the percentage of patients satisfied with their spinal cord implant due to improved pain scores was 84.3%.
SCS is generally a safe procedure. However, some persistent headaches might occur in a patient who has had the spinal cord stimulator placed in the upper cervical spine.
Recently, the implantation of high-frequency SCS at 10 kHz (HF-SCS) has attained conditional approval for MRI, along with retrospective application to earlier implanted devices.
Many patients are discharged from the hospital the same day after the procedure. However, the patient would need the anaesthesia effect to be worn off. The incision sites of the patient may pain for several days post-surgery.
Spinal Cord Stimulator therapy is actually reversible. If at any time the patient decides to terminate the therapy session, the electrical contacts, generator, and wires can all be removed. This results in no permanent variations to the spine.
Metal detectors and other airport devices may detect the patient’s spinal cord stimulator. Due to this, the patient is asked to work with the appropriate agencies to obtain a patient ID card that will help in moving through security checkpoints easily.
Patients who have lighter duty jobs are able to resume work within 6-8 weeks post-surgery. Patients with jobs that require heavy lifting may take slightly longer.